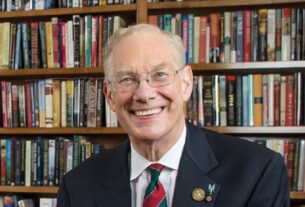
Every day, as Dr. Wendell Parkey enters his clinic in Seminole, a small city on the rural western edge of Texas, he announces his arrival to the staff with an anthem pumping loudly through speakers.
As the song reaches a climax, he throws up an arm and strikes a pose in cowboy boots. “Y’all ready to stomp out disease?” he asks.
Recently, the question has taken on a dark urgency. Seminole Memorial Hospital, where Dr. Parkey has practiced for nearly three decades, has found itself at the center of the largest measles outbreak in the United States since 2019.
Since last month, more than 140 Texas residents, most of whom live in the surrounding Gaines County, have been diagnosed and 20 have been hospitalized. Nine people in a bordering county in New Mexico have also fallen ill.
On Wednesday, local health officials announced that one child had died, the first measles death in the United States in a decade.
It may not be the last. Large swaths of the Mennonite community, an insular Christian group that settled in the area in the 1970s, are unvaccinated and vulnerable to the virus.
The outbreak has struck at a remarkable juncture. Vaccine hesitancy has been rising in the United States for years and accelerated during the coronavirus pandemic. Now the nation’s most prominent vaccine skeptic, Robert F. Kennedy Jr., has been named its top health official, the secretary of health and human services.
Mr. Kennedy has been particularly doubtful of measles as a public health problem, once writing that outbreaks were mostly “fabricated” to send health officials into a panic and fatten the profits of vaccine makers.
At a cabinet meeting on Wednesday, Mr. Kennedy minimized the crisis in West Texas, saying that there had been four outbreaks so far this year (there have been three, according to federal health officials) and 16 last year.
Vaccine fears have run deep in these parts for years, and some public health experts worry that the current outbreak is a glimpse at where much of America is headed. Researchers think of measles as the proverbial canary in a coal mine. It is among the most contagious infectious diseases, and often the first sign that other pathogens may be close behind.
“I’m concerned this is a harbinger of something bigger,” said Dr. Tony Moody, a pediatric infectious disease expert at the Duke University School of Medicine. “Is this simply going to be the first of many stories of vaccine-preventable disease making a resurgence in the United States?”
On the front lines of the outbreak, simple answers aren’t easy to come by.
Measles was officially declared eliminated in the United States in 2000. Not long ago, it had become so rare that many American doctors never saw a case.
But as the outbreak spread, Dr. Parkey learned to spot the signs of infection in the examination room even before he saw the telltale rashes.
School-age children often zipped around the room or pestered their mothers or asked him for lollipops. The children stricken with measles sat still, vacant looks in their eyes.
On Monday, Dr. Parkey walked into a hospital room where an unvaccinated 8-year-old boy sat with that distant stare. His mother had scheduled an appointment after she noticed his barking cough the night before.
By the time they arrived at the clinic, the boy’s eyes were red and crusted. He had a low-grade fever and a blotchy pink rash covering his chest and back.
Dr. Parkey tried the usual banter: “Do you have a girlfriend?” The boy looked past him, glassy eyes trained on the wall.
“Which of your uncles is your favorite?” Dr. Parkey asked. The boy let out a dry cough and slumped further into his seat. He spoke only once, to request a cup of water.
Over the next 24 hours, if the boy’s illness followed the typical progression, he was likely to get sicker. His fever would spike, and the rash would fan out over his torso and thighs.
If he was lucky, the worst would pass within a few days. If he was not, the virus might find its way into his lungs and cause pneumonia, potentially making it difficult breathe without an oxygen mask.
Measles might even invade his brain, causing swelling and possible convulsions, blindness or deafness.
Doctors have few options to alter its course once the virus infects someone. There is no treatment that will stop it, only medicines to make the patient more comfortable.
Dr. Parkey wrote prescriptions for cough syrup and antibiotics for the boy. A nurse swabbed the back of his throat for a sample to be shipped to the state health department in a box of dry ice, adding to the county’s growing case count.
Scary Stories Online
For decades, the doctors at Seminole Memorial Hospital had been having conversations with patients about the importance of childhood vaccines.
Even on busy days with back-to-back appointments, staff members sat down with parents to discuss fears about side effects and to recount the horrors of many preventable diseases.
Go to an old cemetery, Dr. Parkey often told his patients — look at how many children died before vaccines arrived. In many families, though, minds were made up, and the conversations rarely broke through.
The largest school district in Gaines County reported that just 82 percent of kindergartners received the measles, mumps and rubella (M.M.R.) vaccine in 2023. One of the smaller school districts reported that less than half of the students had received the shot.
For a virus as contagious as measles — which spreads through microscopic droplets that can linger in the air for two hours — experts say that at least 95 percent of a community must be vaccinated in order to stave off an outbreak.
Gaines County, a dusty expanse the size of Rhode Island dotted with cotton fields and whirring pump jacks, had not hit that mark in many years.
Although there is no religious doctrine that bans vaccination, the county’s tightknit Mennonites often avoid interacting with the medical system and hold to a long tradition of natural remedies, said Tina Siemens, a Seminole historian who has written several books about the community in West Texas.
In recent years, concerns about childhood vaccines appeared to rise even in the broader Seminole community, especially after Covid-19, several doctors said. An outbreak began to feel inevitable.
“I’d never seen measles, but I knew it was coming,” Dr. Parkey said.
In this respect, Gaines County is not so different from much the country.
Before the pandemic, 95 percent of kindergartners in the United States had received the M.M.R. vaccine, according to federal tallies. The figure sunk below 93 percent last year. Immunization rates against polio, whooping cough and chickenpox fell in similar proportions.
When the cases in Texas first surfaced, local doctors and health officials hoped that the outbreak would make the M.M.R. vaccines an easier sell. If parents saw what measles did to children, the thinking went, they would understand what the vaccine was designed to protect them from.
But there has been no stampede to vaccination. In Seminole, a city of about 7,200 people, almost 200 residents have received shots at pop-up clinics.
“Hopefully, at least the next generation will change their minds about vaccines,” Dr. Parkey said. “Just maybe not this one.”
One mother told Dr. Leila Myrick, a family medicine physician at Seminole Memorial, that the measles outbreak had helped solidify her decision not to vaccinate her children. She’d heard from a friend that the virus was similar to a bad flu.
Even some parents who recognized the dangers that measles posed to their children still felt that vaccines were riskier.
Ansley Klassen, 25, lives in Seminole with her husband and four young children, three of whom are fully unvaccinated. She considered bringing her children to a vaccine clinic when measles cases first started popping up.
Mrs. Klassen, who is about five months pregnant, knew she didn’t want to risk getting measles. She had been scrubbing counters with Lysol wipes and keeping her children away from others as much as possible.
But on social media, she had seen a deluge of frightening posts about the side effects of vaccines: stories of children developing autism after a shot or dying from metal toxicity. (Both claims have been debunked by scientists.)
“There are stories that you can read about people multiple hours after they got the vaccine having effects, and that’s scary to me,” she said. “So I’m like, is it worth the risk? And right now I can’t figure that out.”
These anecdotes — regardless of whether they are factual — are part of what has made vaccine hesitancy such an intractable problem in the age of social media, said Mary Politi, a professor at the Washington University School of Medicine who studies health decision-making.
Stories about children who don’t have serious side effects from vaccines and never contract vaccine-preventible illnesses don’t go viral on TikTok, she noted.
“It’s not that they’re trying to make a bad choice or do something against evidence,” she said. “People are trying to do the best thing they can for their families, and they don’t know who to trust.”
Mrs. Klassen didn’t consider herself staunchly anti-vaccine. Her oldest daughter, now 6, had received all of her vaccines up to a year.
But she didn’t trust everything doctors were telling her, either. She thought the Covid-19 vaccine had been developed too quickly and pushed too forcefully, making her skeptical that the authorities were telling the truth about the measles shot.
She prayed about it and ultimately decided to forgo the vaccine. “The trust I have in the medical system is not there,” she said.
It’s not just unvaccinated people who are at risk during the current outbreak.
Measles increases the likelihood of stillbirths and serious complications in pregnant women, yet they cannot receive the vaccine or booster.
Andrea Ochoa, a nurse’s assistant at Seminole Memorial who is six months into her first pregnancy, said she thought about taking time off from her job but ultimately decided to stay so she could keep her health insurance.
She wore an N95 mask during her entire shift, which sometimes made her so lightheaded that she sat in her car for a break. She showered as soon as she was home.
“I hope it doesn’t get worse,” Ms. Ochoa said of the outbreak. “I don’t know what choice I would make.”
Five vaccinated residents also have contracted measles, state health officials said. At the clinic, Dr. Parkey recently cared for a teacher who was vaccinated but immunocompromised.
A serious measles infection kept the teacher curled in a fetal position on the couch for a week, her eyes so swollen that she opened them only for brief runs to the bathroom, she recalled in an interview. She asked not be named to protect her privacy.
The West Texas measles outbreak is far from the largest in the United States in recent years. In 2019, outbreaks in at least two dozen states sickened more than 1,250 people.
A vast majority of those infections occurred in “underimmunized, close-knit communities,” the C.D.C. noted. More than 930 patients were infected in Orthodox Jewish communities in New York.
Federal, state and local officials swung into action with vaccination campaigns that led to more than 60,000 M.M.R. immunizations in the affected communities. They reached out to religious leaders, local doctors and advocacy groups.
And in areas like Williamsburg, Brooklyn, officials went further, issuing mandates requiring vaccination.
The campaign in West Texas has been less forceful. Management of outbreaks like this one falls to state health officials, and they ask for help from the C.D.C. and other federal resources as necessary.
The C.D.C. is providing some technical assistance, but Texas health officials said they did not need more help from the agency. They have not declared a public health emergency, as officials did in parts of New York State, nor have they moved to mandate vaccination.
“We can’t force anybody to take a drug — that’s assault,” said Dr. Ron Cook, a health official in nearby Lubbock, at a news conference on Friday.
Zachary Holbrooks, the local public health official for four Texas counties, including Gaines, said that type of mandate would be deeply unpopular in the state, where individual freedom is a strongly held value.
Texas public schools require children to have received certain vaccines, including the M.M.R. shot. But in this state, as in many others, parents can apply for an exemption for “reasons of conscience,” including religious beliefs.
In January, as the first cases of measles began spreading in Gaines County, state legislators introduced several bills designed to weaken school vaccination requirements.
“I don’t want to see a baby’s lips turn blue because they can’t breathe,” Mr. Holbrooks said. “I don’t want anybody to suffer from long-lasting disability because they got measles.”
“But if you choose to live in Texas,” he added, “you can exercise that option.”